Rhinology/Allergy
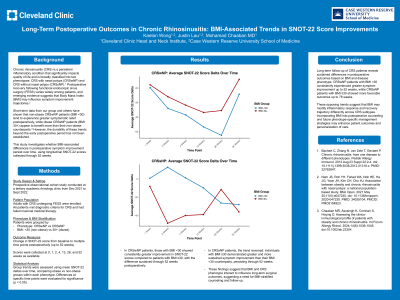
(A1129) Long-Term Postoperative Outcomes in Chronic Rhinosinusitis: BMI-Associated Trends in SNOT-22 Score Improvements
Monday, October 13, 2025
12:00 PM - 1:00 PM EDT
Location: OTO EXPO, Posters
Kaelan Wong, BS
Medical Student
Case Western Reserve University School of Medicine
Cleveland Heights, Ohio, United States- MC
Mohamad Chaaban, MD, MSCR, MBA
Cleveland Clinic
westlake, Ohio, United States
Presenting Author(s)
Senior Author(s)
Disclosure(s):
Kaelan Wong, BS: No relevant relationships to disclose.
Introduction: Body Mass Index (BMI) has been linked to differential postoperative outcomes in chronic rhinosinusitis (CRS). Short-term data suggest better outcomes in CRS with nasal polyps (CRSwNP) for patients with BMI < 30, while the reverse is observed in CRS without nasal polyps (CRSsNP). This study evaluates whether these BMI-associated trends persist in the long term.
Methods: This prospective observational study was conducted from December 2021 to September 2022 and focused on chronic rhinosinusitis (CRS) with and without nasal polyps (CRSwNP and CRSsNP). Subjects included patients undergoing functional endoscopic sinus surgery (FESS) at a tertiary care center, stratified by BMI into two groups: < 30 and ≥30. The primary intervention was FESS, with symptom improvement measured using SNOT-22 scores collected at baseline, early postoperative time points, and follow-ups up to 104 weeks for CRSwNP and 78 weeks for CRSsNP. Independent variables included BMI group, CRS phenotype, and time since surgery. Preliminary analyses examined trends in SNOT-22 score deltas over time to evaluate long-term postoperative outcomes.
Results: In the CRSwNP group, patients with BMI < 30 demonstrated greater long-term improvements in SNOT-22 scores compared to those with BMI ≥30, with this trend persisting up to 104 weeks. Conversely, in the CRSsNP group, patients with BMI ≥30 experienced greater symptom improvements than those with BMI < 30, with trends sustained up to 78 weeks. These findings align with prior short-term observations and confirm the role of BMI in influencing postoperative outcomes in CRS patients.
Conclusions: This study demonstrates sustained BMI-associated differences in postoperative outcomes for CRS patients. CRSwNP patients with BMI < 30 exhibit better long-term improvements in SNOT-22 scores compared to those with BMI ≥30, while the reverse is observed in CRSsNP patients. These findings highlight the importance of considering BMI as a factor in predicting postoperative recovery and underscore the need for further research into the underlying mechanisms driving these trends.
