Head and Neck Surgery
(A555) Immune Checkpoint Inhibitors and Venous Thromboembolism in Patients with Head and Neck Cancer Undergoing Surgery
Monday, October 13, 2025
12:00 PM - 1:00 PM EDT
Location: OTO EXPO, Posters
- FM
Febronia Morcos Mansour, BS
Medical Student
SUNY Upstate Medical University
Syracuse, New York, United States - KA
Komal Akhtar, MD
SUNY Upstate, United States
- KA
Kiranya E. Arnold, MD
SUNY Upstate
Syracuse, New York, United States
Presenting Author(s)
Co-Author(s)
Senior Author(s)
Disclosure(s):
Febronia Morcos Mansour, BS: No relevant relationships to disclose.
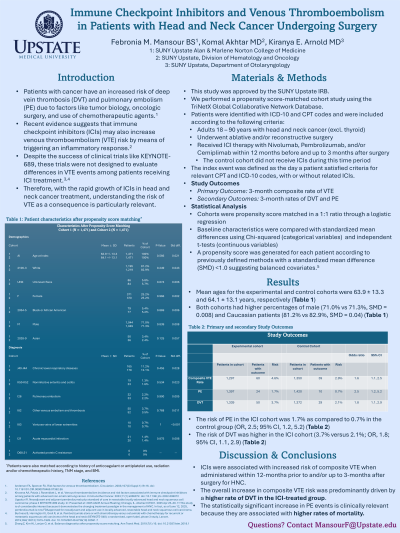
Introduction: Perioperative venous thromboembolism (VTE) is associated with significant morbidity. Although this risk is multifactorial, recent studies suggest immune checkpoint inhibitors (ICIs) may also contribute to increased VTE risk. However, little is known about the risk of VTE and use of ICIs in patients undergoing surgery for head and neck cancer (HNC). The aim of this study is to evaluate VTE risk in a cohort of patients with HNC treated with surgery and ICIs.
Methods: De-identified data from the TriNetX Global Collaborative Network database was used to identify adult surgical patients (≥18 years) using International Classification of Diseases 10th Revision and Common Procedural Terminology codes and were further refined by use of nivolumab, pembrolizumab, or cemiplimab within 1-year before or up to 3-months after surgery. Cohorts were propensity score matched and the primary study outcome was the 3-month composite rate of VTE (PE and DVT).
Results: After propensity score matching, there were 1,471 patients in each cohort and they were well balanced according to demographics, body mass index, comorbidities, medication use, and radiation history up to 1-year before the index event. The composite rate of VTE in the study population was 3.74% and was higher in patients treated with ICIs (4.63% versus 2.89%; OR, 1.63; 95% CI, 1.08, 2.46). The rate of PE (1.72% versus 0.70%; OR, 2.47; 95% CI, 1.17, 5.17) and DVT (3.73% versus 2.11%; OR, 1.80; 95% CI, 1.13, 2.86) were higher in the ICI group when compared to the control group.
Conclusions: This study highlights the importance of risk stratification and adequate risk reduction in the setting of increasing ICI use for patients with HNC undergoing surgery.
