Sleep Medicine
(A1218) Racial and Socioeconomic Disparities in Surgical Outcomes for Obstructive Sleep Apnea: A Scoping Review
Monday, October 13, 2025
12:00 PM - 1:00 PM EDT
Location: OTO EXPO, Posters

Tenesha Kelly Boyd, MHS
Medical student
Meharry Medical College
Nashville , Tennessee, United States- SS
Shumit Saha, PhD
Meharry Medical College, United States
Presenting Author(s)
Senior Author(s)
Disclosure(s):
Tenesha Kelly Boyd, BS, MBS: No relevant relationships to disclose.
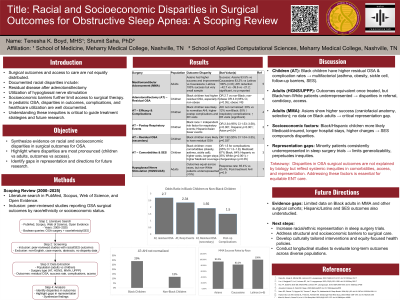
Introduction: Racial and socioeconomic disparities in surgical outcomes for obstructive sleep apnea (OSA) pose significant challenges to equitable healthcare. This scoping review explores how systemic and socioeconomic factors influence OSA surgical success, recovery, and post-operative adherence, while identifying gaps in the existing research.
Methods: Peer-reviewed studies published from 2020 were identified through comprehensive searches in PubMed, Scopus, and Web of Science. Inclusion criteria focused on studies reporting OSA treatment outcomes across racial groups, particularly surgical interventions. Studies without racial data were excluded. Data extraction included participant demographics, treatment modalities (e.g., adenotonsillectomy, maxillomandibular advancement), outcomes (residual OSA, adherence), and disparities. A thematic analysis was conducted to identify patterns and gaps in the literature.
Results: Six studies revealed significant inequities, particularly among Black patients. Black children had higher residual OSA rates post-adenotonsillectomy, especially in non-obese cases (Fayson et al., Pediatrics, 2023). Black adults experienced slower recovery and lower adherence to post-operative care, reflecting systemic barriers (Stewart et al., JCSM, 2023; Smith et al., Sleep Medicine, 2023). Controlling for socioeconomic factors reduced these disparities, highlighting structural inequities as a major driver (Williams et al., Annals of Surgery, 2023). Advanced therapies were similarly effective across racial groups, but non-White participants were underrepresented, indicating access issues (Khan et al., Sleep, 2022).
Conclusions: This review highlights the importance of addressing socioeconomic barriers and implementing tailored interventions to ensure equitable OSA surgical outcomes.
